Best Practice: Infection Control – Blood Collection
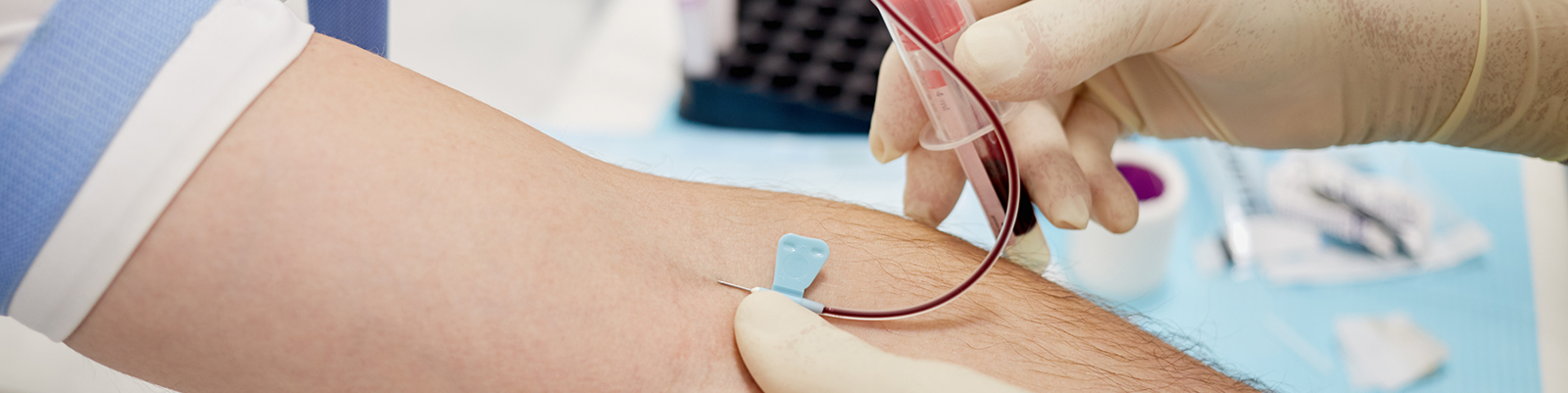
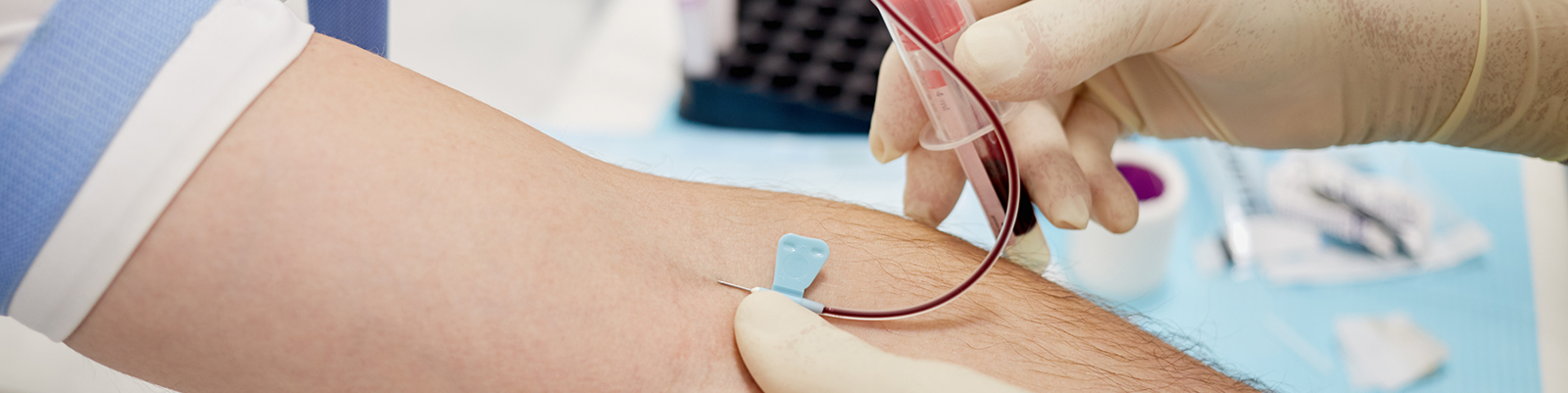
According to the World Health Organization guidelines, these are the best practice guidelines for blood collection in order to prevent the spread of infection:
Best practice DO’s
• DO carry out the correct hand hygiene procedure before and after each patient.
• DO use one pair of sterile gloves per procedure or patient.
• DO use a single-use device for blood sampling.
• DO use a clean tourniquet reprocessed between patients.
• DO disinfect the skin at the venepuncture site.
• DO use a closed vacuum system for blood sampling.
• DO discard the used device immediately into a sharps container.
• DO seal the sharps container with a tamper-proof lid.
• DO immediately report any incident linked to a sharp injury and seek assistance.
Best practice DO NOT’s
• DO NOT forget to clean your hands.
• DO NOT use the same pair of gloves for more than one patient.
• DO NOT wash gloves for reuse.
• DO NOT use a needle, lancet or vacutainer for more than one patient.
• DO NOT use a visibly dirty or unprocessed tourniquet between patients.
• DO NOT touch the puncture site after disinfecting it.
• DO NOT use needles and syringes to take blood or inject blood into laboratory tubes.
• DO NOT leave an unprotected needle lying outside the sharps container.
• DO NOT overfill or decant a sharps container.
• DO NOT delay seeking assistance after exposure to potentially contaminated material; beyond 72 hours, Post-exposure Prophylaxis is NOT effective.
Health care professionals & training
To reduce the risk of adverse effects for patients, health workers undertaking phlebotomy need to be trained in procedures specific to the types of specimen they collect.
All healthcare workers should receive immunisation for hepatitis B before assuming duties that include potential exposure to blood and body fluids.
The environment
All blood collection procedures should be taken in a dedicated location that ensure patient comfort and privacy, and that allows best practice standards to be met. The dedicated area should include:
• A clean surface area
• 2 chairs (one for the phlebotomist and one for the patient)
• A hand wash basin with soap, running water and paper towels
• Alcohol hand rub
Floors should not be carpeted and in general the workplace should be clean and tidy with no sign of blood contamination on any of the surface areas.
To remove the risk of environmental contamination and prevent infection, surfaces and chairs should be cleaned with disinfectant at the start of each shift and when visibly dirty.
A post-exposure prophylaxis protocol must be available in all phlebotomy areas, providing clear instructions to follow in case of accidental exposure to blood or body fluids.
What equipment can help me prevent infection when collecting blood?
All items designed to be used on more than one patient should be designed so that they can easily be cleaned and disinfected between uses. Equipment needed include:
• Sterile, single-use blood-sampling devices should be used to take blood.
The use of vacuum extraction tube systems as closed systems for blood collection reduces the risk of direct exposure to blood and has made it easier to take multiple samples from a single venepuncture.
• A clean tray or trolley should be used to lay out equipment.
• Non-sterile gloves in a range of sizes.
• Gauze or cotton-wool ball for application over the puncture site.
• Alcohol swabs for skin preparation.
• Tourniquet.
Use a clean elastic tourniquet reprocessed between patients.
• Leak proof transportation bags and containers.
• A puncture resistant sharps container.
PPE & hand hygiene
When taking blood, health workers should wear well fitting, non-sterile gloves and should also carry out a full hand hygiene procedure before and after each patient, before putting on gloves and after removing them. Our handy guide to correct hand washing practices can help ensure you a washing correctly.
Skin preparation
To ensure the patients skin is sterilised health workers should clean the whole area with an alcohol swab, ensuring that the skin area is in contact with the disinfectant for at least 30 seconds; they should then allow the area to dry completely (about 30 seconds). DO NOT touch the cleaned site; in particular, DO NOT place a finger over the vein to guide the shaft of the exposed needles. If the site is touched, repeat the disinfection.
Sharps safety
A thorough sharps safety procedure is vital for limiting the risk of infection spreading. Best practice is to discard the needle and tube holder, as a single unit, into a puncture resistant sharps container that us clearly visible and within arm’s reach.
Dangerous practices with should be avoided include:
• Recapping and disassembling vacuum-containing tubes and holders.
• Reusing tourniquets and vacuum-tube holder that may be contaminated with bacteria and blood.
• Working alone with confused or disoriented patients who may move unexpectedly.




