Dental



“Great things are never done by one person. They’re done by a team of people.” (Steve Jobs)
As a collective, Brosch Direct and Polyco Healthline staff have chosen to give back to the community by taking 4 MILLION steps in April to raise funds and awareness for Don’t lose hope, a local Bourne charity.
4 million steps to spotlight and promote the three components of well-being: comfort, happiness and health.
The pressure is ever upon us, and everybody needs a method to cope with the ‘normal’ stresses of daily life, but on occasions you may feel restricted and overwhelmed – at times like these, you are not alone.
Don’t lose hope, is a group of highly experienced professionals offering group or individual counselling services for the

Whether you're the office first aider, or just a conscious employee we all know the purpose of first aid kits

To ensure your disinfectant is effective it should have achieved the following standards...

In the world fight against Coronavirus surface cleaning and disinfection is essential in preventing the spread of the virus...

Evans have put together this helpful guide to talk you through the differences between cleaning, disinfecting and sanitising products to ensure you are using the correct product for the job.

Face masks are effective at preventing the spread of coronavirus but only if they are worn correctly. Follow our handy steps below to make sure you are staying safe and protected by using them in the corret way.
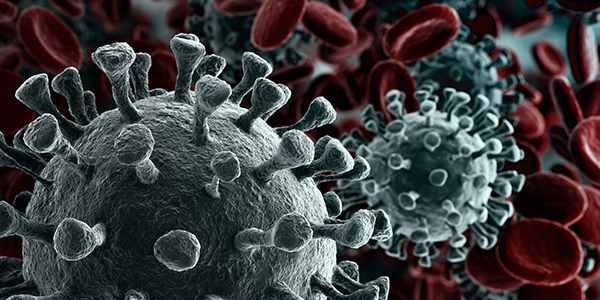
Here are what our leading hand hygiene and disinfectant product suppliers have to say about the effectiveness of their products against the coronavirus bacteria...

When selecting the right disposable gloves for the task at hand, there is a surprising amount you need to consider. Here we have broken down each type of disposable glove avalable, plus what each one is best for and why, into an easy to follow guide...

Here, Brosch Direct breaks down how to put on disposable gloves to ensure you can go about tasks safely and with minimal risk. This step-by-step breakdown should reduce the likelihood of workplace incidents occurring and ensure your business is covered...

The removal of gloves may appear to be a simple task. However, when working in environments where cross contamination must be avoided and infection is a risk, it’s important the correct removal procedures are carried out...

Introducing robust infection control procedures are undoubtedly the most import way to prevent cross contamination. Addressing infection control issues and introducing infection control measures is vital in all care homes, businesses and public areas as well as healthcare settings...



